Within the world of substance abuse and the subsequent treatment, co-occurring disorders are one of the greatest concerns. A co-occurring disorder is any disorder that exists concurrent, or at the same time as a substance use disorder. The National Eating Disorder Association (NEDA) reports research finding that up to 50% of individuals experiencing an eating disorder also have a substance use disorder.
Understanding Anorexia Nervosa
Anorexia nervosa (AN) most commonly arises in adolescence or the teen years, and can carry onwards to a person’s adult life. More common in women, it can also affect men. Recently, the criteria as set forth by the Diagnostic and Statistical Manual of Mental Disorders has changed, with the publication of their 5th edition. The criteria for anorexia nervosa, as extracted from American Family Physician, is:
- Restriction of energy intake relative to requirements, leading to a significantly low body weight in the context of age, sex, developmental trajectory, and physical health. Significantly low weight is defined as a weight that is less than minimally normal or, for children and adolescents, less than that minimally expected.
- Intense fear of gaining weight or of becoming fat, or persistent behavior that interferes with weight gain, even though at a significantly low weight.
- Disturbance in the way in which one’s body weight or shape is experienced, undue influence of body weight or shape on self-evaluation, or persistent lack of recognition of the seriousness of the current low body weight.
According to NEDA, there are two subtypes of anorexia:
Binge-Eating/Purging Type — If within the last three months, the person exhibited behaviors of binging (eating excessive amounts of food, more than is considered a meal, in a short period of time) and/or purging (a person makes themselves pass food they consumed, either by self-induced vomiting, or by using laxative, dietetics, or other harmful methods.)
Restricting Type — A person’s actions do not involve the above patterns of behaviors.
 One of the biggest changes between the DSM-IV and DSM-V criteria, is the criterion that dealt with body weight. Now geared more towards recognizing this eating disorder as a physiological one, rather than only a weight disorder, these new guidelines broaden the scope of access for those who need help.
One of the biggest changes between the DSM-IV and DSM-V criteria, is the criterion that dealt with body weight. Now geared more towards recognizing this eating disorder as a physiological one, rather than only a weight disorder, these new guidelines broaden the scope of access for those who need help.
Signs Someone Has Anorexia And/Or Substance Abuse
When a person suffers from anorexia, they often develop idiosyncratic behaviors surrounding mealtimes and their eating habits. For instance they may exhibit any of the following:
- Substantial weight loss
- Loss of period
- Eating mainly fruits, vegetables, and diet food products
- Developing food rituals (dabbing excess oils or liquids off food, cutting food into tiny bites, or rearranging food on their plate)
- Becoming adamant about not eating certain types or groups of food
- Overly concerned with weight, caloric intake, fat content, and dieting
- Expressing worry about being “fat,” or about gaining weight
- Ignoring that they’re hungry
- Always having a reason to be absent during meals
- Exercising in an extreme manner in an attempt to offset caloric intake
- The preoccupation and mindset concerning eating, dieting, food intake, and weight lost shift to a person’s primary focus.
If a person is struggling with a drug or alcohol addiction, you may witness them:
- Exhibiting secretive behavior, including hiding drugs or alcohol
- Lying about their drug or alcohol use
- Becoming unable to stop drinking or using, even if they want to
- Requiring more and more of the substance to feel the same way they used to feel
- Letting their responsibilities slip, whether they be work, school, or family related
- Not taking care of their appearance or grooming
- Taking risks or doing things they normally wouldn’t
- Having relationship troubles
- Continuing to use even when faced with the damaging consequences
- Exhibiting withdrawal if they stop using drugs or alcohol
Some characteristics or behaviors may be suggestive of either anorexia or substance abuse, such as withdrawing from their family and friends, losing interest in activities that they previously enjoyed, or having mood swings.
The Connection Between Anorexia And Substance Abuse
Eating disorders are widely linked to substance abuse, and anorexia nervosa is no different. Many instances of abuse and addiction arise out of an individual’s desire to self-medicate a variety of symptoms, including mental health needs. As various mental health disorders are common in individuals with AN, they may quickly resort to substances as a means to treat these or for emotional regulation.
Caffeine and nicotine are commonly abused substances by individuals who have anorexia, because they are appetite suppressants. People may use amphetamines or methamphetamine to expedite their weight loss, only to find that their abuse becomes an addiction. Individuals who exhibit purging characteristics may abuse laxatives or diuretics to further this behavior. It has been found that alcohol abuse and addiction are more common in AN which exhibits binging and/or purging behaviors. People may use marijuana to cope with the stress they feel from both their lives and this hidden disorder.
One startling practice that is becoming especially widespread in college students, is termed “drunkorexia.” Though not always associated with anorexia, this dangerous habits is sometimes used by those with this disorder. In essence, drunkorexia is essentially the behaviors of anorexia or bulimia combined with alcohol abuse, especially binge drinking. A person may not eat, or exercise excessively, with the knowledge that they intend on drinking heavily in the near future.
Dangers Of These Combined Disorders
Standing alone, these disorders are dangerous in and of themselves, together, the danger skyrockets, leading a person down a path of physical decline. These are some results:
Slowed cardiovascular system — Anorexia causes a person’s heart functions and muscle structure to become altered, leading to decreased heart rate and blood pressure. Various types of substance abuse and overdose can also cause this, further increasing the risk of heart failure that may be present for those with AN.
Malnourishment — Clearly, as a person fails to consume adequate amounts of food, their body struggles to maintain critical body systems and processes as it fails to find the nutrients, vitamins, and chemicals it needs; anemia may occur. Malnourishment is common in most all instances of substance abuse. Alcohol, inhalants, and opioids are examples of drugs that can cause anemia.
Depleted bone density — Because of the malnourishment, a person may get osteoporosis, leading to brittle and dry bones. Heavy drinking may cause this, and research suggests that opiate addictions can as well.
Extreme dehydration — Anorexia can severely dehydrate a person, the extent that they get kidney failure. Many drugs of abuse lead to dehydration, most notably perhaps is an alcohol addiction, which can also cause kidney failure. MDMA (ecstasy) can also lead to these concerns.
Muscle depletion and weakness — Without proper nutrients, a person’s body cannot build and maintain muscle mass. Muscle atrophy can result from an alcohol addiction. Cocaine may also lead a person’s muscle tissue to break down and amphetamines may cause muscle weakness.
Weakness marked by fatigue or fainting — Without caloric intake and the essential nutritional and chemical compounds that are found in food, an individual with AN has little means to make energy. These symptoms are also widely prevalent in many drugs of abuse.
Dry hair and skin — Again, due to a lack of nutrients, a person’s body cannot upkeep itself. A person may even begin to lose hair. Various drugs of abuse may also deplete a person’s body in the way that their hair and skin begin to show wear, especially alcohol abuse.
Body hair growth — As a person loses their critical fat stores, they may grow a downy type of hair called lanugo as their body attempts to warm itself.
Anorexia can be deadly, giving credence to the phrase “starving yourself to death,” a risk that is further compounded by substance abuse or addiction. Reports cite that out of every mental illness, anorexia has the highest mortality rate, finding that 4% of those with this disorder will die due to complications of the disease, whereas others say 20% when including suicide. Due to a reported 56 times greater likelihood of committing suicide, one in five of these deaths is attributed to suicide. Coupled with the toll of drug or alcohol, this risk may be even higher.
How Are Eating Disorders And Substance Abuse Similar?
Why does a person develop an eating disorder? The scientific community recognizes it may be due to several things, including environmental, biological, and psychosocial influences. What is interesting, is that within both eating and substance use disorders, persons may encounter some of the same feelings that lead them to these behaviors/disorders, such as:
- Depression
- Social or generalized anxiety
- Urge to self-medicate
- Addictive personality
- Family dysfunction
Some researchers even suggest that eating disorders are in and of themselves addictions, as explained by an article presented in Psychiatric Times, as these “individuals typically require more of the behavior to produce the same reinforcing effect,” and have been found to have cravings, continue their harmful behaviors despite the apparent danger of their ways, and exhibit significant instances of relapse.
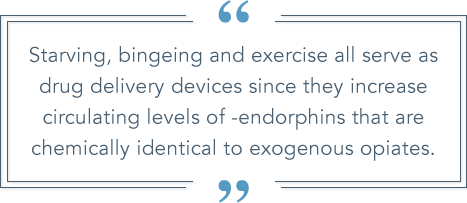
These parallels continue on a biological level too—the article notes that “starvation activate the dopaminergic (DA) reward pathway of the brain. The resulting biological events underlie the auto-addiction opioid theory, which proposes that a chronic eating disorder is an addiction to the body’s production of endogenous opioids and therefore is identical to the physiology and psychology of substance abuse in general. In other words, starving, bingeing and exercise all serve as drug delivery devices since they increase circulating levels of -endorphins that are chemically identical to exogenous opiates, and these endorphins are as potentially addictive because of their ability to stimulate DA in the brain’s mesolimbic reward centers.”
Though this might seem overwhelming, these parallels may make treatment for these co-occurring disorders in some ways more efficient as certain modules may work simultaneously and succinctly for certain aspects of both disorders.
Treating These Co-Occurring Disorders
The best rehab facility for these concerns is one that is adept at treating each need. Due to the severity of these co-occurring disorders, generally, an inpatient drug rehab program would be recommend, due the residential format and the longer around of time that it allows a person to receive treatment. In extreme cases, hospitalization or a feeding tube may be required.
During treatment, a person may first receive a medical detox, to rid their body of the drug. Medical supervision is especially important during this time because of the increased fragile nature of their body and mind due to AN. They may then receive nutritional and vitamin supplementation to help them recover from both the eating disorder and the substance abuse or addiction. Treatment may entail individual, group, or family sessions, and various forms of psychotherapies. If a person has any physical health concerns resulting from these co-morbid conditions, these will need to be treated at this time as well.
Cognitive behavioral therapy is an excellent, evidenced-based treatment for both AN and substance use disorders. When considering therapy, your support team will also look to any other co-occurring disorders like depression and anxiety which may aggravate these disorders, that may need to be treated as well.
Medication-supported treatment can have a crucial role within treatment for both disorders. The Oxford published article, “Recognizing alcohol and drug abuse in patients with eating disorders,” asserts that naltrexone may work for eating disorders and concerns of alcohol addiction, and that some research leads scientists to think that serotonin reuptake inhibitors (SSRIs) may also work for both.
We Can Help You On The Path To Better Self-Care And Sobriety
 We realize that individually, these disorders may be daunting and when combined, they may be hugely overwhelming, however, we also firmly believe that with the proper team behind you and perseverance, you can be treated. If you’re struggling with one or both of these, DrugRehab.org is standing by to help you find the caliber of care that is best suited to your unique health needs. Contact us for compassionate help today.
We realize that individually, these disorders may be daunting and when combined, they may be hugely overwhelming, however, we also firmly believe that with the proper team behind you and perseverance, you can be treated. If you’re struggling with one or both of these, DrugRehab.org is standing by to help you find the caliber of care that is best suited to your unique health needs. Contact us for compassionate help today.
Sources
National Association of Anorexia Nervosa and Associated Disorders — Eating Disorder Statistics
American Family Physician — Initial Evaluation, Diagnosis, and Treatment of Anorexia Nervosa and Bulimia Nervosa
Mirror Mirror — Eating Disorders Statistics
National Eating Disorder Association — Anorexia Nervosa
Social Work Today — Insatiable Hungers: Eating Disorders and Substance Abuse
